End-of-life planning is simply the process of making your wishes clear for your medical care, finances, and personal affairs. This isn't about giving up. Far from it. It's an incredible act of love that provides clarity and comfort for your family when things get tough.
Think of it as creating a personal roadmap for your loved ones to follow.
Why End of Life Planning Is an Act of Love
Let's be honest: many of us put off end-of-life planning because it feels uncomfortable, maybe even a little morbid. It forces us to think about our own mortality, a topic most would rather avoid.
But it helps to reframe the process. Instead of seeing it as preparing for an end, think of it as creating the ultimate user manual for your wishes. This guide gives your family the incredible gift of certainty right when they need it most.
Taking these steps now prevents confusion, potential family arguments, and a mountain of stress down the road. When your wishes are clearly documented, your loved ones are freed from the awful burden of guessing what you would have wanted. They can focus on supporting each other and honoring you, rather than trying to navigate complex legal and medical decisions in the middle of a crisis.
This is the ultimate way to ensure your voice is heard and your family is protected from uncertainty. By taking control now, you provide peace of mind for yourself and those you care about most.
The Core Components of Your Plan
A truly effective plan touches on several key areas, each playing a vital role in painting a complete picture of what you want. Tackling these components ensures that every aspect of your life is managed exactly to your preferences.
The main elements we'll walk through in this guide are:
- Medical Directives: These are the legal documents that spell out your preferences for medical treatments. They also name a specific person to make healthcare decisions for you if you become unable to.
- Financial and Estate Arrangements: This covers everything from wills and trusts to handling your digital assets, making sure your legacy is passed on smoothly and without headaches.
- Personal Wishes: This is where you can include instructions for your memorial service, how you want your pets cared for, and any other personal details that are important to you.
Getting a handle on these pieces is the first big step toward building a solid plan. As you consider long-term care, you might also want to look into different living arrangements. To better understand one common option, you can learn more about what is assisted living and see how it fits into a bigger care strategy. This whole process is an empowering journey that protects your independence and your family.
Making Your Medical Wishes Clear With Advance Directives
When it comes to your health, your voice is the most important one in the room. But what happens if you’re suddenly unable to speak for yourself? This is where advance directives become absolutely essential tools in your end of life planning journey.
Think of them as legally binding documents that clearly outline your preferences for medical care. They ensure your wishes are heard and respected even when you can’t communicate them.
I know, thinking about these scenarios is tough. But failing to plan can create immense stress and heartbreaking conflict for your loved ones. Without your guidance, families are often left guessing, which can lead to painful disagreements during an already traumatic time. Advance directives remove that uncertainty. They provide a clear roadmap for your medical care that aligns with your values.
This proactive step is more critical than you might think. Globally, less than 30% of individuals have actually documented their end-of-life care preferences. This leaves the vast majority of people without a clear voice in their final days.
This simple flowchart helps visualize why planning is a crucial step for everyone, regardless of their family situation.
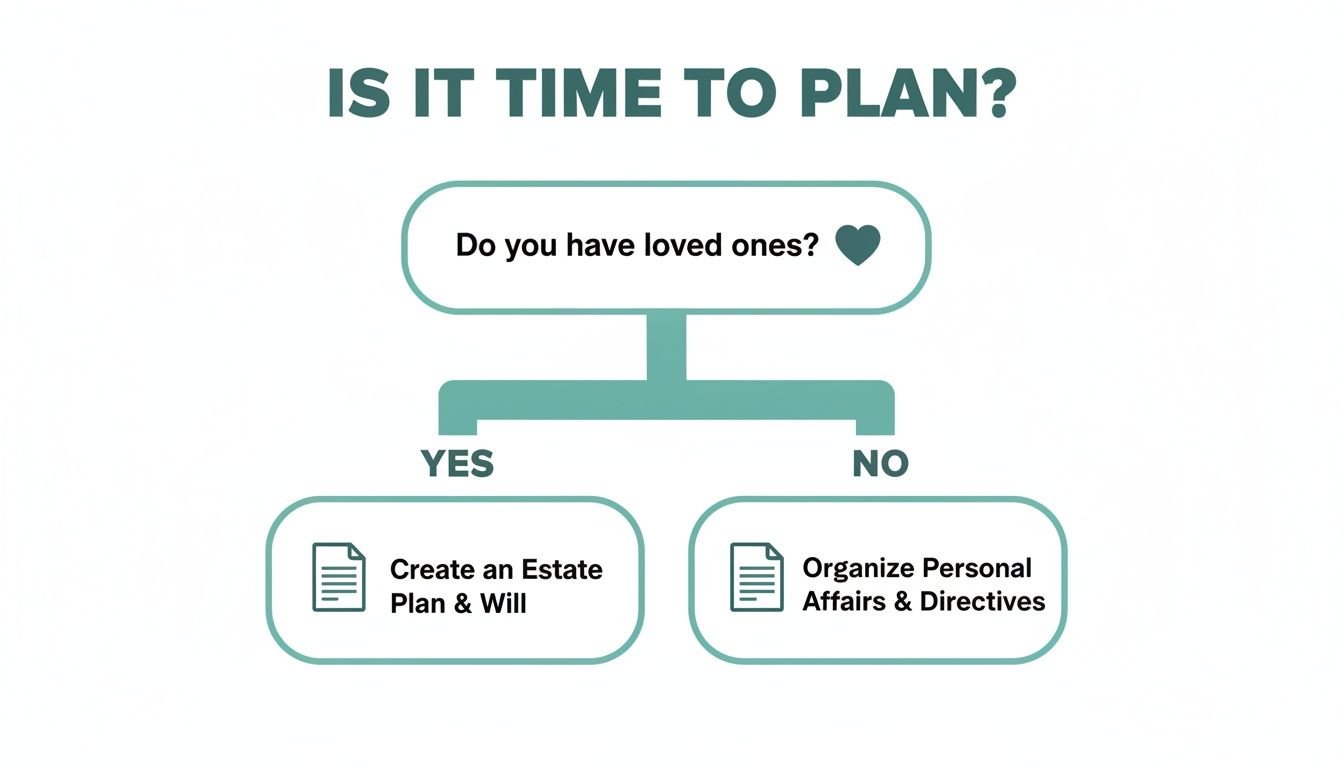
The key takeaway is this: having loved ones makes formal planning essential to protect them, while having no immediate family makes it vital to protect yourself.
Your Healthcare Co-Pilot: The Durable Power of Attorney
Imagine you’re the pilot of your own healthcare journey. A Durable Power of Attorney for Health Care (sometimes called a healthcare proxy or agent) is like appointing a trusted co-pilot. This is the person legally empowered to make medical decisions on your behalf if you become incapacitated.
Your co-pilot doesn’t take over the controls unless you're unable to fly the plane yourself. You choose this person—a trusted family member, a close friend—who truly understands your values and promises to advocate for your wishes. Without one, decisions could be left to a court-appointed guardian or lead to disputes among family members who disagree on the best course of action.
Your Flight Plan: The Living Will
If the durable power of attorney is your co-pilot, then your Living Will is your flight plan. This document details your specific instructions regarding medical treatments you would or would not want to prolong your life.
A living will addresses those difficult situations where you might be terminally ill or permanently unconscious. It answers critical questions about life-sustaining treatments, such as:
- Mechanical Ventilation: Do you want a machine to breathe for you if you cannot breathe on your own?
- Tube Feeding: If you are unable to eat, do you want to receive nutrition and hydration through a tube?
- Dialysis: Do you want to undergo this procedure if your kidneys fail?
This document speaks for you, making sure your deeply personal choices about medical intervention are honored. For a comprehensive overview, this guide explains exactly what an advance directive entails.
Understanding Specific Medical Orders
While a living will outlines your general preferences, some situations require more immediate, specific instructions that medical professionals can follow instantly. This is where documents like DNR and POLST orders come into play. They aren't just planning documents; they are actionable medical orders.
To make these different documents easier to understand, let's break down the key medical planning documents in a simple table.
Comparing Key Medical Planning Documents
| Document | Primary Purpose | When It's Used |
|---|---|---|
| Living Will | Outlines your general wishes for end-of-life medical treatment. | When you are terminally ill or permanently unconscious and cannot communicate. |
| Durable Power of Attorney | Appoints a person (your agent) to make healthcare decisions for you. | Anytime you are unable to make or communicate your own medical decisions. |
| DNR Order | Instructs medical staff not to perform CPR if your heart or breathing stops. | In a medical emergency, typically for someone with a terminal illness. |
| POLST Form | Translates your wishes into specific medical orders for emergency responders. | For individuals with a serious advanced illness, effective across all care settings. |
Each document serves a unique and vital role in ensuring your healthcare journey reflects your personal values.
A Do Not Resuscitate (DNR) Order is a very specific medical order. It tells healthcare providers not to perform cardiopulmonary resuscitation (CPR) if your heart or breathing stops. This is a choice some people with a terminal illness make to avoid aggressive, often invasive, interventions at the very end of life.
A Physician Orders for Life-Sustaining Treatment (POLST) form is more detailed than a DNR. It's a medical order for those with serious advanced illnesses that translates your wishes into concrete actions for emergency personnel. It covers your preferences for CPR, medical interventions like intubation, and artificially administered nutrition.
Once you've created these vital documents, the final step is distribution. Your appointed healthcare agent, your primary care physician, and any specialists you see should all have copies. It’s also wise to give copies to close family members. Keep the original in a safe but accessible place—not a bank safe deposit box that can't be opened on a weekend. This ensures everyone on your care team is on the same page, ready to honor your wishes with clarity and confidence.
Securing Your Legacy Through Estate Planning

While advance directives take care of your medical wishes, estate planning is all about securing your financial legacy. More than that, it protects your family from a world of administrative headaches down the road. This part of end of life planning is much more than just writing a will; it's a complete strategy for managing everything you own, both during your life and after you’re gone.
Let's be honest—the financial side of planning can feel intimidating. But it doesn't have to be. If you approach it with a clear roadmap, what seems like a massive task becomes a series of small, manageable steps. This preparation is a final act of love, making sure your assets go where you want them to and saving your family from stress and potential arguments.
It’s clear people are taking this more seriously than ever. The end-of-life planning market was recently valued at a staggering $33.62 billion and is expected to climb to $52.04 billion within five years. That surge is happening for a reason: people want guidance to navigate rising healthcare costs and an uncertain economy, showing just how important this act of care has become.
Wills and Trusts: The Cornerstones of Your Plan
The two biggest tools in your estate planning toolbox are the will and the trust. People often talk about them in the same breath, but they do very different jobs. It helps to think of it this way.
A will is like a detailed letter of instruction you leave behind. It’s a legal document spelling out exactly who should get your property and assets after you pass away. If you have young children, this is also where you’ll name a guardian to care for them. The catch? A will only kicks in after you’re gone and has to go through a court process called probate, which can be slow and is completely public.
A trust, on the other hand, is like a secure container you create to hold your assets while you're still here. You can put things like your house, investments, and bank accounts into the trust, which is then managed by a person you choose (a trustee) for the people you name (your beneficiaries). The biggest advantage is that assets in a trust usually get to skip probate, meaning a faster, private transfer to your family.
Appointing Your Financial Advocate
Just like you need someone to make medical decisions if you can't, you also need a financial advocate. This is where a Durable Power of Attorney for Finances comes in. This document gives a trusted person the legal authority to manage your money—pay your bills, handle investments, file taxes—if you become incapacitated.
Choosing this person, often called your agent, is a huge decision. It needs to be someone responsible, organized, and completely committed to acting in your best interest. Without one, your family could face a long, expensive court battle just to get a guardian appointed to manage your affairs.
A Durable Power of Attorney for Finances isn't just for end-of-life planning. It’s a critical safeguard for any unexpected life event, ensuring your financial world stays on track even when your health doesn't.
The Overlooked Details: Beneficiaries and Digital Assets
Modern estate planning has a few new wrinkles. Two areas that are easy to forget but can cause massive problems are beneficiary designations and digital assets.
Many of your financial accounts—like life insurance, 401(k)s, and IRAs—let you name a beneficiary directly on the account. These designations are incredibly powerful because they override whatever is in your will. You absolutely have to review these accounts regularly, especially after big life changes like a marriage, divorce, or a new baby, to make sure the right person is still listed.
And in today's world, we all have a sprawling collection of digital assets. This is everything from online bank accounts and social media profiles to cloud-stored photos and emails. Creating a digital estate plan isn't optional anymore; it's a necessity.
Your Essential Document Checklist
One of the best first steps you can take is simply gathering all your important documents into one spot. It makes the process easier for you now and is a massive help to your executor later on.
- Property Documents: Deeds for your home or any other real estate.
- Vehicle Titles: The titles for your cars, boats, or RVs.
- Financial Statements: Recent statements for all bank accounts, investment portfolios, and retirement funds.
- Insurance Policies: Life insurance, homeowners insurance, and any long-term care policies. Thinking about future care means you need to understand your long-term care insurance coverage for assisted living, as it's a vital piece of the financial puzzle.
- Tax Returns: Copies of your federal and state tax returns from the last few years.
- Digital Asset Inventory: A secure list of your online accounts with usernames and instructions (but always store passwords separately and safely).
Getting your financial life organized is a profound gift to your family. It gives them a clear roadmap, lifts a huge administrative weight off their shoulders, and lets them focus on what truly matters: honoring you.
Understanding Comfort Care: Hospice and Palliative Options
Facing a serious illness is one of life’s biggest challenges. A compassionate end of life planning process involves knowing all your options, especially two that are often misunderstood: palliative care and hospice care. They both prioritize comfort and quality of life, but they serve different needs at different times.
Think of palliative care as an extra layer of support you can bring in at any point after a serious diagnosis. It doesn't replace treatment; it works right alongside it. The goal is simple: to relieve the symptoms, pain, and stress that a complex medical condition brings, making the entire journey more manageable.
Hospice care, on the other hand, comes into play when the focus shifts away from curative treatments and entirely toward comfort and peace. It’s not about giving up. It’s about choosing to live your final months with dignity, surrounded by a team dedicated to your well-being.
Palliative Care: A Support System for the Journey
Imagine you’re on a long, tough road trip. Palliative care is like having an expert support crew riding with you. This team—often doctors, nurses, and social workers—helps smooth out the bumps in the road like pain, nausea, and anxiety. They make sure you can continue your journey with as much comfort as possible.
You can receive palliative care in a hospital, a clinic, or right in your own home. The most important thing to remember is that you can get this support while still undergoing aggressive treatments like chemotherapy. The two work together to care for the whole person.
Hospice: A Focus on Comfort and Dignity
Hospice is for the final leg of that journey. It typically begins when a doctor confirms that a person likely has six months or less to live if the illness follows its natural course. At this stage, the goals change from curing the disease to making sure the time you have left is peaceful and comfortable.
The hospice team provides a huge range of services, not just for the patient but for the whole family. They’re there to meet physical, emotional, and spiritual needs.
This support often includes:
- Expert Pain and Symptom Management: Using specialized techniques to keep someone comfortable without sacrificing alertness.
- Emotional and Spiritual Counseling: Offering support for the person nearing life’s end and for their loved ones navigating this difficult time.
- Medical Equipment and Supplies: Taking care of practical needs like hospital beds, oxygen, and other items for home-based care.
- Respite for Caregivers: Giving family caregivers a much-needed break to rest and recharge.
It’s a holistic approach designed to honor a person’s final wishes and create a supportive environment for everyone involved.
A common misconception is that entering hospice means giving up hope. In reality, it is a powerful choice to redefine hope—shifting it from a hope for a cure to a hope for peace, comfort, and quality time with loved ones.
Choosing this path gives you more control over your final chapter, allowing it to unfold in a familiar, comforting setting. For families wondering how this works within a senior living community, learning about hospice care in assisted living can show how this comfort-focused support is seamlessly integrated. Ultimately, this decision is about making sure your final months are lived on your own terms.
Introducing the Role of an End of Life Doula
Beyond the medical teams and even dedicated family members, a vital new role is emerging in the world of end of life planning: the end-of-life doula. You might also hear them called death doulas.
These are non-medical companions who provide emotional, spiritual, and practical support to people and their families during the final stages of life.

Think of a doula as a guide for one of life’s most profound transitions. While doctors and nurses are focused on physical health, a doula’s attention is on the person’s holistic well-being. They step in to fill the gaps that often appear in traditional care, prioritizing personal connection, dignity, and peace.
The need for this kind of compassionate presence is growing fast as conversations around death become less taboo. For instance, the National End of Life Doula Alliance (NEDA) in the US ballooned from just 260 members to over 1,500 in only a few years. Meanwhile, the International End of Life Doula Association (INELDA) has already trained 8,000 doulas worldwide.
This trend highlights a major need, especially when you consider that only 14% of people who require palliative care globally actually receive it. You can learn more about this important movement and discover why dying well is a key trend.
What a Doula Can Offer You and Your Family
The support an end-of-life doula provides is deeply personal and flexes to fit each unique situation. Their work isn’t about medical tasks but about creating a supportive atmosphere that honors the individual's journey.
Their services often include:
- Legacy Work: Helping create tangible memories, like writing letters, putting together photo albums, or recording life stories to leave for loved ones.
- Vigil Planning: Assisting the family in preparing for the final days and hours, creating a calm and sacred space that reflects the person's wishes.
- Respite for Caregivers: Giving family members a much-needed break to rest and recharge, knowing their loved one is in caring hands.
- A Calming Presence: Sometimes, it’s as simple as sitting with someone, offering companionship, listening without judgment, and providing comfort just by being there.
An end-of-life doula serves as an advocate for the dying person's non-medical wishes, ensuring their voice is heard and their final chapter is filled with dignity and compassion.
Bridging the Gap in End of Life Care
Having a doula can dramatically change the end-of-life experience for everyone involved. They serve as a neutral, supportive figure who can help navigate complex family dynamics and tough emotional conversations. By focusing on the emotional and spiritual side of dying, they beautifully complement the work of the medical team.
For example, a doula might gently help a family understand the physical signs of the dying process, which can demystify the experience and reduce fear. They can also facilitate conversations about what a "good death" looks like for the individual, making sure those final wishes are clearly communicated and honored.
This dedicated support helps transform a time of potential fear and chaos into a period of meaningful connection and peace.
How to Start the Conversation with Your Family
Bringing up end-of-life planning is often the biggest hurdle families face. The whole topic feels heavy, and it's easy to put it off because of how emotional it can be. But if you can frame it as an act of love—a way to make sure wishes are always honored—it can go from being a dreaded task to a moment that brings everyone closer.
The key is to be gentle and intentional. You definitely don't want to ambush family members during a holiday dinner or some other stressful time. It's much better to pick a calm, private moment when nobody feels rushed or put on the spot.
Setting the Right Tone
Just getting the conversation started is half the battle. You can ease into it with a gentle, non-threatening opener that centers on being practical and caring, rather than on finality. The goal is to make it feel like a team effort, not a grim announcement.
Here are a few gentle ways to begin:
- "I was reading an article about planning for the future, and it got me thinking. It seems like a smart idea for us to get everything organized. Can we set aside some time to talk about it?"
- "It would give me so much peace of mind to know that you both understand my wishes. I never want you to be in a position where you have to guess what I'd want."
- "Remember what happened with [friend's family]? It really showed me how important it is to have these conversations before we have to."
Framing this discussion as a gift to your loved ones—the gift of clarity—helps take away the fear. It's about empowering them to act confidently for you, not burdening them with a tough subject.
Navigating the Discussion with Empathy
Once the conversation is underway, expect some emotions. It's completely normal for family members to feel sad, anxious, or even try to shut down the topic. Your role is to listen with an open heart and validate their feelings without letting the conversation get derailed.
Acknowledge how they're feeling by saying something like, "I know this is hard to talk about, and I really appreciate you being here with me." Just showing that you understand can help everyone feel heard and respected. Make sure to write down the key decisions and wishes that come out of these talks.
These conversations can be draining for everyone, especially for the primary caregiver. Having a plan for some backup support can make a world of difference. Looking into options like what is respite care can give caregivers a much-needed break while knowing their loved one is still in great hands. This isn't a one-and-done conversation; it's a journey, so be patient with yourself and your family.
Common Questions About End of Life Planning
Even when you have a good handle on things, questions are bound to pop up during the end of life planning process. Think of this section as a quick FAQ, hitting on the common sticking points that can trip people up. Getting these answers can give you the confidence to move forward.
One of the first questions people ask is, "When should I start?" The simplest answer is right now. This kind of planning isn't just for older adults or someone with a serious diagnosis. An unexpected accident or health scare can happen to anyone, which makes it so important for every adult to have their wishes written down.
Cost is another big worry. People often assume that creating a plan means racking up expensive legal bills. While it’s always a good idea to bring in an attorney for complicated financial situations, you can often complete foundational documents, like an advance directive, using low-cost or even free forms your state provides.
Can I Change My Mind Later?
Of course. An end-of-life plan isn't a one-and-done deal. It’s a living document that should change as your life does. It’s a good habit to pull out your documents for a review every few years or whenever something big happens.
Here are a few key moments that should trigger a review:
- A change in marital status: Getting married, divorced, or becoming widowed.
- A significant health diagnosis: Receiving a new diagnosis for yourself or the person you chose as your healthcare agent.
- Changes in your family: The birth of a child, the death of a beneficiary, or if a named agent can no longer serve.
- A major financial shift: A big jump or drop in your assets.
Treat your plan like a personal roadmap—you can always update the route if your destination changes. This keeps your documents perfectly aligned with your current wishes.
What If My Family Disagrees with My Choices?
This is a very real fear, and it’s exactly why having clear, legally sound documents is so critical. When your wishes are spelled out in a living will or a durable power of attorney, they carry legal authority. These documents are designed to make sure your choices are respected, even if family members feel differently.
Having honest conversations with your loved ones now can also head off conflicts down the road. Explaining why you made certain decisions helps them understand your point of view, making it easier for them to support you when the time comes. If you need a more structured way to tackle this, an essential end-of-life planning checklist can give you clear steps to follow.
Another practical question that comes up is how to pay for long-term care. Many families wonder about financial help, and figuring out details like whether assisted living is covered by Medicaid is a huge piece of the puzzle. Answering these financial questions now can lift a massive weight off your family’s shoulders later on.
At Forest Cottage Senior Care, we know that planning for the future brings up a lot of important decisions. Our team is here to offer guidance and support as you look at different senior living options. Visit us online to learn how we can help you or your loved one start a brighter, more supported chapter.