When you first step into the role of a dementia caregiver, it can feel like the world has shifted on its axis. It’s a journey filled with complex emotions and new practical demands that completely reshape your day-to-day life. You're not just managing symptoms; you're caring for a whole person whose reality is fundamentally changing. Just acknowledging how hard this is going to be is a crucial first step toward building a care plan that works—for both of you.

This isn’t just a private family challenge anymore. Globally, dementia care is now recognized as a major public health issue. Back in 2019, the worldwide cost of dementia was a staggering US$1.3 trillion. Think about that. And what’s even more eye-opening is that about half of that cost was shouldered by family and friends providing informal care.
These are the unsung heroes—people like you—who give an average of five hours of care and supervision every single day. Recognizing this massive contribution, global initiatives, like those from the World Health Organization, are now pushing for systems that support not just the person with dementia, but their caregivers, too.
The Four Pillars of Effective Dementia Care
To keep from feeling completely overwhelmed, it helps to break down your approach into four core areas. I think of these as the foundational pillars that will hold up your entire caregiving strategy, giving you a framework to lean on when new challenges pop up.
To give you a quick roadmap, here are the core areas we'll be diving into. Think of this table as your starting point for building a strong, sustainable caregiving plan.
| Pillar of Care | Key Objective | Simple First Step |
|---|---|---|
| Understanding the Condition | To anticipate needs and respond with informed compassion. | Read a short article about the specific type of dementia your loved one has. |
| Creating a Supportive Environment | To reduce anxiety and confusion through safety and routine. | Walk through your home and identify one or two simple safety changes, like removing a tripping hazard. |
| Communicating with Empathy | To connect and validate feelings when words fail. | Practice using simple, direct sentences and a calm, reassuring tone of voice. |
| Prioritizing Your Wellbeing | To prevent burnout so you can provide consistent, loving care. | Identify one person you can call for support or to vent for just 10 minutes this week. |
Let's unpack what these pillars really mean in your day-to-day life.
Understanding the Condition: You can’t fight an enemy you don’t know. Learning about the specific type of dementia your loved one has—its stages, its quirks, its likely path—is your best weapon. Knowledge turns frustration into informed compassion.
Creating a Supportive Environment: A calm, predictable space is a gift to someone with dementia. It drastically cuts down on their anxiety and confusion. This means more than just safety-proofing; it’s about creating steady daily routines for meals, hygiene, and other activities of daily living.
Communicating with Empathy: When dementia scrambles language and logic, you have to learn a new way to communicate. Forget about correcting mistakes. Focus on body language, use simple words, and validate their feelings. The connection is more important than the facts.
Prioritizing Your Wellbeing: This is the pillar that caregivers let crumble first, and it’s the most dangerous one to lose. Burnout is real, and it’s destructive. You simply cannot pour from an empty cup. Making time for your own health—through rest, support systems, and respite—isn’t selfish. It’s essential.
The most important thing to remember is that you are not on this journey alone. Reaching out for help from support groups, friends, and professional services is a sign of incredible strength, not weakness.
Creating a Safe and Structured Home
As dementia progresses, the world changes for your loved one. Their own home, once a place of comfort and familiarity, can suddenly feel confusing, stressful, and even dangerous. Learning how to care for someone with dementia means seeing the world through their eyes and thoughtfully redesigning their environment to match.
The focus shifts to safety, simplicity, and a predictable structure.

This isn't just about making physical changes; it's about creating a world they can navigate with confidence. Much like memory care communities are intentionally designed to support residents, your own home can become a sanctuary. The goal is simple: build a space that reduces agitation and promotes well-being.
Modifying the Home for Physical Safety
First things first, you need to do a complete safety sweep of the home. You have to look at every room with a new perspective, imagining the potential hazards for someone with cognitive and physical challenges. Even the smallest adjustments can prevent a serious accident.
Start with the most common culprits. Tripping hazards are a huge one, so get on your hands and knees and look for loose rugs, stray electrical cords, and general clutter. Securing or removing these things clears the way for safer movement.
Here are a few key modifications to consider, room by room:
- Living Areas: Open up the space by removing extra furniture that isn't essential. Make sure the lighting is bright and even—shadows can easily be misinterpreted and cause fear.
- Kitchen: Install safety knobs on the stove and get in the habit of unplugging appliances like the microwave when they're not in use. It's also crucial to lock away sharp objects, medications, and cleaning supplies.
- Bathroom: This is a high-risk area for falls. Install grab bars by the toilet and inside the shower, lay down non-slip mats, and—this is important—turn the water heater down to below 120°F (49°C) to prevent scalding burns.
- Bedroom: A simple nightlight between the bedroom and bathroom can make a world of difference. Consider a lower bed or one with safety rails to help prevent falls during the night.
For an extra layer of security, modern technology can be a huge help. It might be worth learning more about how senior monitoring systems can provide solutions like fall detection and wandering alerts, which bring invaluable peace of mind for caregivers.
The Power of Routine and Structure
Beyond making the physical space safe, a predictable daily routine is probably the single most powerful tool you have. When short-term memory is unreliable, a consistent schedule acts as an anchor, giving the day a sense of purpose and security.
A structured day helps orient someone who can no longer track time. It answers the unspoken question, "What happens next?" This predictability minimizes confusion and can dramatically reduce agitation, especially in the late afternoon when "sundowning" often occurs.
A stable routine is not about rigidity; it's about reliability. The goal is to create a familiar rhythm for meals, activities, and rest that your loved one can depend on, which helps them feel safe and grounded in their own home.
Building a Calming and Navigable Space
As cognitive abilities decline, just getting around the house becomes a challenge. Simple visual cues can be a game-changer, helping your loved one maintain their independence and cutting down on frustration for everyone.
Think about how you can make the environment easier to understand.
- Use Labels: Put simple, clear labels on drawers and cabinets, maybe with both words and pictures (e.g., "Socks," "Plates"). This empowers them to find what they need.
- Contrast Colors: A brightly colored toilet seat stands out against a white floor, making it easier to see. Using a contrasting placemat can help define their eating space at the table.
- Reduce Confusion: Cover up mirrors if the reflection is causing distress. It's common for a person with dementia to not recognize themselves and think a stranger is in the room. Likewise, busy patterns on wallpaper or curtains can be overwhelming; solid, calming colors are much better.
For instance, if your loved one often gets lost on the way to the bathroom at night, try leaving the bathroom light on with the door slightly ajar. These small adjustments empower them to function more independently and with greater confidence. By adapting the home, you're doing more than just preventing accidents—you're creating a space that is truly supportive.
Communicating and Managing Behavioral Changes
Connecting with someone living with dementia often feels like learning a new language—one built not on words, but on patience, empathy, and intuition. As their ability to process information shifts, your communication style has to adapt right along with it. This isn't just a nice-to-have skill; it's the foundation of compassionate care.

It’s truly more about how you say something than what you actually say. A calm, gentle tone can work wonders where even the most perfectly chosen words fall flat. Simple, direct sentences are much easier for them to grasp than complex questions or long-winded explanations.
Mastering Empathetic Communication
When conversations become difficult, it helps to remember that your loved one is almost always trying to express a need or an emotion, even if it doesn't come out that way. Your role shifts to that of a detective, looking for the feeling hidden behind their words (or lack thereof).
Here are a few practical techniques that can make a real difference in your daily interactions:
- Approach Gently: Always try to approach from the front and make eye contact before you start talking. This small step prevents startling them and shows you're giving them your undivided attention.
- Keep It Simple: Stick to one idea at a time. Instead of asking, "Would you like to put on your sweater and then go for a walk?" try, "Let's put on your sweater." Once that's done, you can suggest the next thing.
- Lean on Non-Verbal Cues: A warm smile, a gentle touch on the arm, or a reassuring nod can communicate care and understanding when words fail. Your body language often speaks volumes.
- Listen with Your Eyes: Pay close attention to their gestures and facial expressions. If they seem upset, you can say something like, "It looks like you're feeling sad." This validates what they're feeling and shows you're truly trying to connect.
It’s so important to avoid arguing or correcting them about facts. If they say they're waiting for a parent who passed away years ago, arguing will only cause more confusion and distress. Their reality is different now, and validating their emotional state is far more important than being factually right.
Understanding and Responding to Behavioral Changes
Changes in behavior like agitation, repetition, or wandering aren't intentional acts of defiance. Think of them as a form of communication—an expression of an unmet need. The real key is to figure out the cause. Are they hungry? In pain? Bored, lonely, or feeling overwhelmed?
Remember, all behavior is communication. Instead of reacting to the action itself, try to understand what your loved one is trying to tell you. This shift in perspective can transform a frustrating situation into a moment of connection.
Take "sundowning," for example—that period of increased confusion and agitation that often kicks in late in the afternoon. This isn't random. It can be triggered by fatigue, low light creating confusing shadows, or a disruption to their internal clock. A compassionate response might be to close the curtains, turn on some soft lights, and play calming music before that time of day even arrives.
Consistent, hands-on support is the bedrock of good dementia care. A major cross-national study found that at least 1 in 5 people with dementia get no help at all with basic daily activities. Researchers discovered this gap in care was directly linked to higher risks of ER visits, depression, and even premature death. It’s a heavy burden, with women globally shouldering about 70% of dementia care hours. You can read more about this global study on dementia care to understand the full impact.
When faced with challenging behaviors, it's easy to feel lost. The table below offers some common scenarios and compassionate ways to respond by looking for the need behind the action.
Responding to Common Dementia Behaviors
| Behavior | Potential Cause (Unmet Need) | Compassionate Response Strategy |
|---|---|---|
| Repetitive Questioning | Anxiety, insecurity, memory loss | Answer calmly each time. Offer reassurance. Write the answer down on a notepad for them to see. |
| Agitation/Restlessness | Pain, boredom, overstimulation | Reduce noise/clutter. Play calming music. Go for a slow walk. Check for physical discomfort. |
| Wandering | Need for exercise, confusion, looking for something familiar | Ensure a safe environment with locked doors. Go on supervised walks. Create a "rummage box" with safe, interesting items. |
| Refusing to Bathe | Fear of water, feeling cold, loss of privacy, feeling controlled | Use a gentle tone, explain each step, ensure the room is warm, use a handheld shower, and respect their dignity. |
| "I want to go home." | Feeling insecure, lost, or uncomfortable | Avoid arguing. Validate their feeling: "I know you want to go home. Tell me about your favorite room there." Redirect with a snack or favorite activity. |
These strategies aren't about "fixing" the behavior but about meeting the person where they are with kindness and understanding. It's a process of trial and error, so be patient with yourself and with them.
Strategies for De-escalation and Redirection
When your loved one becomes agitated, your calm presence is your most powerful tool. It's tough, but try to avoid raising your voice or showing your own frustration. Instead, gently redirect their attention to something pleasant and familiar.
For instance, if they are repeatedly asking to "go home" while sitting in their own living room, they are likely expressing a need for security and comfort, not a literal desire to leave. Instead of correcting them, you could say, "This place does feel different sometimes, doesn't it? Tell me about your childhood home."
Meaningful engagement is a fantastic redirection tool. It provides a sense of purpose and can soothe an anxious mind. Our guide on https://www.forestcottageseniorcare.com/activities-for-seniors-in-assisted-living/ has tons of simple ideas you can adapt for home, from listening to their favorite old songs to folding laundry together. Even the presence of a gentle therapy animal, like the Goldendoodle at Forest Cottage, can have a profoundly calming effect. The goal is always to shift their focus from the source of anxiety to an activity that brings comfort and a touch of joy.
Navigating Medical and Financial Responsibilities
When you’re caring for someone with dementia, your role often expands beyond day-to-day emotional and physical support. You quickly find yourself stepping into the complex worlds of medical coordination and financial planning. It can feel like a lot to take on, but getting these areas organized is one of the most powerful and loving things you can do for your family member.
Think of yourself as the central hub for their entire care team. You become the person connecting the dots between the neurologist, the primary care physician, and the pharmacist. This role is absolutely critical for making sure everyone is on the same page, preventing dangerous medication mix-ups, and effectively advocating for your loved one, especially as they lose the ability to speak for themselves.
Organizing Medical Care and Appointments
One of the first, most practical things you can do is create a central place for all medical information. A simple three-ring binder or even a dedicated folder on your computer can become your caregiving command center. This binder should be the one thing you can grab for any appointment or emergency.
Make sure it includes these key documents:
- Contact List: A straightforward list of all doctors, specialists, and pharmacies with their phone numbers and addresses.
- Medication Schedule: A detailed log of every medication—dosages, when they’re taken, and which doctor prescribed them. Be sure to note any side effects you notice.
- Medical History: A summary of major health conditions, past surgeries, and any known allergies.
- Appointment Log: A section where you can jot down notes during visits—what was discussed, any new instructions, and questions you want to ask next time.
Having this system in place ensures nothing gets missed and empowers you to be a confident and prepared advocate.
During an appointment, never hesitate to ask for clarification until you feel 100% comfortable with the information. Repeating instructions back to the doctor is a simple trick that can prevent critical mistakes with medications or treatment plans.
Tackling Legal and Financial Planning Early
Talking about legal and financial matters can feel awkward, but it's a conversation you absolutely cannot afford to put off. It's so important to have these discussions and get legal documents signed while your loved one still has the cognitive ability to participate in the decisions. A crucial first step is to understand what a Power of Attorney document really grants.
These documents aren’t about taking control away; they’re about honoring your loved one’s wishes when they can no longer voice them. The key documents to get in place include:
- Power of Attorney (POA) for Finances: This lets a designated person manage financial tasks like paying bills and handling bank accounts.
- Power of Attorney (POA) for Healthcare: This appoints someone to make medical decisions on their behalf.
- Living Will or Advance Directive: This document outlines their wishes for end-of-life care, such as their feelings on life-sustaining treatments.
Putting these plans in place provides legal authority and clarity, which can prevent family arguments and stressful court battles down the road. For more compassionate guidance on these sensitive talks, check out our guide on end-of-life planning.
Understanding the Long-Term Costs of Care
The financial reality of dementia care can be a shock, which is why planning ahead is so vital. The total annual cost is staggering, and families often end up shouldering a huge portion of that expense.
The numbers really highlight why a plan is non-negotiable. Families and individuals pay an estimated $52 billion out-of-pocket for dementia-related costs each year. These figures show why structured support like respite stays, medication management programs, and eventually assisted living can be such a crucial lifeline for caregivers.
Support and Resources for Veterans
For families of veterans, there are specific benefits that can offer significant financial relief. The Department of Veterans Affairs (VA) has programs like Aid and Attendance, which can help pay for the costs of long-term care, including assisted living.
Navigating the VA system can be a real headache, but you don't have to do it alone. Organizations like Forest Cottage specialize in helping families understand and apply for the benefits their loved ones have earned. We can guide you through the paperwork and help ensure your family receives the support they rightfully deserve for their service.
How to Avoid Caregiver Burnout
You’ve probably heard the old saying, "you can't pour from an empty cup." In dementia care, this isn't just a cliché; it's a fundamental truth. Prioritizing your own well-being isn't selfish. It's an absolute requirement if you want to provide sustainable, patient, and loving support to your family member.
Ignoring your own needs doesn't just hurt you—it ultimately chips away at the quality of care you're able to give.
Caregiver burnout is a state of total exhaustion—physical, emotional, and mental. It has a way of creeping in slowly, marked by a growing sense of detachment and the feeling that your entire life has been swallowed by your caregiving role. Recognizing it is the first step toward finding balance again.
Identifying the Early Warning Signs
Burnout shows up in different ways, and the signs can be pretty subtle at first. Maybe you notice you’re more irritable than usual or you’re having trouble sleeping even when you feel bone-tired. You might even feel a sense of dread about the day ahead. It’s so important to pay attention to these shifts.
Common signs that burnout is creeping in include:
- Physical and Emotional Exhaustion: Feeling tired all the time, getting sick more often, or noticing changes in your sleep or appetite.
- Increased Irritability or Anxiety: Finding yourself snapping over small things, feeling constantly worried, or struggling with new or worsening anxiety.
- Social Withdrawal: You start turning down invitations from friends or feel too drained to connect with family. It's a growing sense of isolation from everything outside of caregiving.
- Loss of Interest: Hobbies and activities that you used to love just don't seem interesting or fulfilling anymore.
Learning to recognize the signs of emotional burnout before they become overwhelming is a critical skill. It lets you take action before you hit a wall.
Practical Strategies for Self-Care
When you’re a dementia caregiver, self-care isn't about spa days or long vacations. It’s about weaving small, intentional moments of rest and recovery into your daily and weekly routine. Think of these small acts as investments in your own resilience.
A great place to start is by asking for—and actually accepting—help. This is often the hardest step for caregivers, but it’s a sign of strength, not failure. Whether it's a friend who can sit with your loved one for an hour while you take a walk or a family member who can run errands, delegating even small tasks can make a world of difference.
Seeking support is not admitting defeat. It's actively managing your resources so you can keep providing the best possible care. You are your loved one's most valuable asset—protect that asset fiercely.
Leveraging Respite Care and Support Systems
Sometimes, an hour off just isn't enough. There will be times when you need a real, substantial break, and that’s where professional support systems become absolute lifelines.
Adult day programs and respite care services are specifically designed to give you that break. They allow you to rest, recharge, and focus on your own life for a while, knowing your family member is in a safe, engaging environment. Learning more about how respite care for family caregivers can be used strategically is a crucial part of any long-term care plan.
Here at Forest Cottage, we see it firsthand. These breaks enable caregivers to return to their role with renewed energy and patience. It’s a vital service that supports the entire family, ensuring the caregiving journey is manageable for the long haul—without you having to sacrifice your own health in the process.
Deciding When to Transition to Professional Care
Making the move to an assisted living or memory care community is, without a doubt, one of the toughest and most emotionally loaded decisions a family can make. It’s so easy to get tangled up in feelings of guilt, like you're somehow failing your loved one.
But it’s critical to see this for what it truly is. This isn't giving up. It's shifting your role to ensure your loved one gets the specialized support, safety, and quality of life they deserve—and that you get the support you need, too.
Sometimes, the realization that it’s time for a change comes on slowly, a gradual accumulation of small incidents. Other times, a sudden crisis makes the need undeniable. The key is to recognize when the demands of care at home have surpassed what you can realistically and safely provide. This isn't an admission of defeat; it's a profound act of love.
Recognizing the Tipping Points
There are usually clear signs that professional care is the right next step. These tipping points almost always circle back to three things: safety, escalating medical needs, and the caregiver's own well-being.
Ask yourself these hard questions:
- Is home safety a constant worry? Has wandering become a real threat? Are you living in fear of falls, medication mix-ups, or what might happen if they're left alone for even a few minutes?
- Have their medical needs become too complex? Are they requiring care like injections, wound management, or mobility support that you just aren't trained for?
- Has your own health taken a nosedive? Are you dealing with chronic exhaustion, stress-induced illnesses, or depression? You simply cannot pour from an empty cup.
Ignoring your own needs isn't noble; it's unsustainable. As this decision tree shows, prioritizing your own well-being is essential to avoiding burnout.
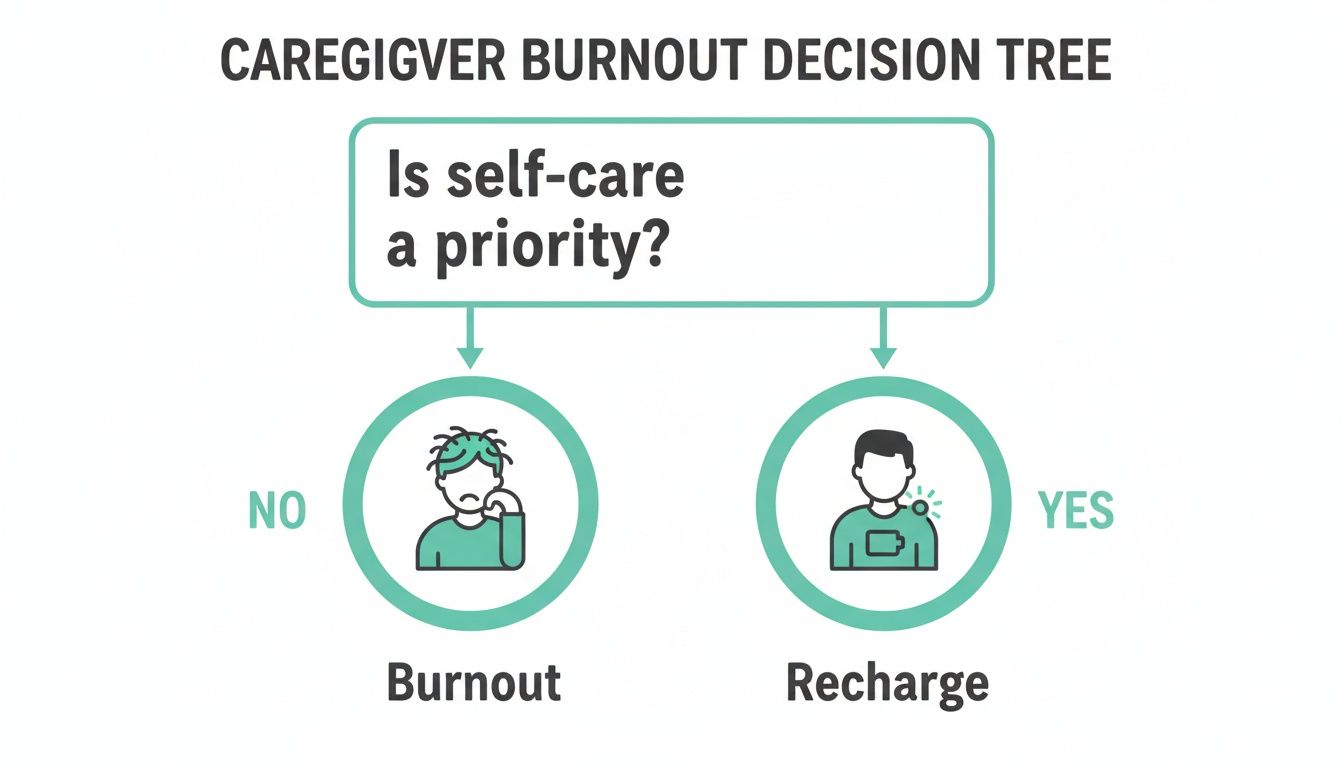
The graphic makes it plain: when you don't make self-care a priority, caregiver burnout isn't just a possibility—it's the destination. And that directly impacts the quality of care your loved one receives.
Choosing the Right Community
Once you start looking at communities, the goal is to find a place that actually feels like a home, not just a facility. When you tour a place like Forest Cottage in Willis, TX, look past the amenities on the brochure. Watch how the staff interacts with the residents. That's where the truth lies.
A warm, engaged staff and happy, calm residents are the most important signs of a high-quality community. Look for genuine connection, not just routine task-completion.
On your tour, get specific with your questions. Ask about staff-to-resident ratios, what kind of dementia-specific training the team receives, and their strategies for handling challenging behaviors. A truly great community will have clear, compassionate answers and will welcome every single question. They get it. They know this is a huge decision, and they'll be there to support you through it.
Common Questions About Dementia Care
When you first step into the world of dementia care, the questions can feel endless and overwhelming. Here are some straightforward answers to the tricky, real-world situations that families tell us they face every single day.
Is It Okay to Lie to Someone with Dementia?
This is a tough one, and it goes against every instinct we have. But in the world of dementia care, sometimes the most compassionate answer is yes. While honesty is always our starting point, sticking to the literal truth can be unintentionally cruel.
Think about it this way: if your mother is in a memory care community and asks when she can go home, reminding her that she no longer lives in her old house can force her to relive that loss over and over again.
Professionals often call this a "therapeutic fib." The goal isn't to deceive, but to protect your loved one from unnecessary pain. Instead of correcting a factual error, try to connect with the emotion behind their words. For example, if they're asking for a parent who passed away years ago, what they're really expressing is a need for safety and comfort.
Instead of arguing about facts, validate the feeling. You could try saying, "It sounds like you really miss him. Tell me about him." This shifts the focus from a painful reality to a cherished memory, meeting their emotional need right where they are.
How Do I Handle Repetitive Questions?
Being asked the same question a dozen times in an hour is one of the most draining parts of caregiving. This behavior isn't intentional; it's a direct result of severe short-term memory loss. Often, it's also fueled by an underlying anxiety or a simple need for reassurance.
The best approach is to answer calmly each time, as if it's the first time you've heard it. Showing frustration will only make them more anxious, which can make the behavior worse.
- Offer Reassurance: The question might just be their way of asking for comfort. A gentle touch on the arm and a warm, calm response can often soothe the anxiety that's driving the repetition.
- Use Visual Cues: Sometimes, seeing is believing. Try writing the answer on a small whiteboard. If they keep asking when Dad is visiting, you can write "Dad is coming at 3 PM" and simply point to it when they ask again.
- Gently Redirect: After you answer, try to shift their attention to something simple and pleasant. You could say, "Dad will be here at 3 PM. How about we listen to some of your favorite music while we wait for him?"
What if They Refuse to Bathe or Change Clothes?
Resistance to bathing and other personal care routines is incredibly common. The reasons can be complex—it could be a fear of falling on a wet floor, feeling cold and exposed, embarrassment, or simply not understanding why it’s necessary anymore.
Trying to force the issue is almost guaranteed to backfire and can lead to what's known as a "catastrophic reaction." Patience and strategy are your best friends here. Make sure the bathroom is warm and cozy. Lay out their clothes ahead of time. Talk them through each step in a simple, reassuring voice.
Sometimes, offering a small choice can make a big difference by giving them a sense of control. For example, "Would you like to wear the blue shirt or the red one today?" And if they still refuse? Just let it go for now. Often, trying again in an hour or so is the most effective solution of all.
Navigating these daily challenges can feel incredibly isolating. At Forest Cottage Senior Care, our team is specially trained in these compassionate, person-first approaches to dementia care. We're here to provide a safe, supportive, and understanding home when you need it most. Learn more about our memory care services.