When you're caring for someone with dementia, it feels like you're running a marathon that never ends. It’s a journey filled with love, no doubt, but it's also incredibly demanding, both physically and emotionally.
Just like a runner needs a water break to keep going, caregivers need a chance to catch their breath. That's exactly what respite care for dementia patients is all about—a planned, temporary break to rest and recharge.
Why Respite Care Is a Lifeline, Not a Luxury
Many families wrestle with guilt when they think about asking for help. It’s easy to feel like you’re somehow failing or giving up. But the truth is, taking a break is one of the most strategic and loving things you can do.
It’s about preventing caregiver burnout, a very real state of physical and emotional exhaustion. Pushing yourself to the brink doesn't make you a better caregiver; it just puts you on a fast track to being unable to provide care at all.
Understanding the Growing Need for Support
This isn't a niche problem—it's a growing reality for millions. The global market for elderly respite care is expected to hit USD 527.1 million by 2032, and people with dementia represent over 40% of that need.
In the U.S. alone, there are more than 11 million people providing unpaid care for a loved one with dementia. These numbers tell a clear story: caregivers need and deserve support.
Let's break down what respite care really provides.
Quick Overview of Respite Care for Dementia
Here's a simple table to summarize the key aspects of what respite care offers.
| Aspect | Brief Description |
|---|---|
| Primary Goal | Provides a temporary break for primary caregivers. |
| Duration | Can range from a few hours a day to several weeks at a time. |
| Setting | Offered in-home, at adult day centers, or in residential communities. |
| Focus for Patient | Safe, professional care with social and cognitive engagement. |
| Focus for Caregiver | Time to rest, handle personal tasks, and prevent burnout. |
| Key Benefit | Sustains the long-term health of both the caregiver and the care recipient. |
This isn't about giving up; it's about setting up a sustainable support system.
Respite as a Tool for Better Caregiving
Think of respite care as a vital tool in your caregiving kit, not an escape. It creates a positive ripple effect for everyone.
- For You, the Caregiver: You get that essential time to sleep, see friends, go to a doctor's appointment, or just sit in a quiet room for a bit. It’s crucial for managing stress and feeling like yourself again.
- For Your Loved One: They get a change of pace and a chance to interact with new people. Good respite programs offer structured activities designed to engage them safely and appropriately.
- For Your Relationship: Taking a small step back allows you to step back in as a spouse, child, or partner—not just a 24/7 caregiver. It can help preserve the warmth and love in your relationship.
Ultimately, respite care helps you stay the course for the long haul. It gives you the strength to return to your role with more patience, energy, and a fresh perspective. Exploring options for temporary senior care is a proactive step toward a better quality of life—for both of you.
Exploring Your Respite Care Options
Once you've realized you need a break, the next step is figuring out what kind of help is out there. Respite care for someone with dementia isn't a one-size-fits-all deal. Think of it as a menu of services designed to fit different family needs, schedules, and personalities. The key is to find the option that feels right for your loved one and your unique situation.
Let's walk through the three main ways you can get that much-needed relief. Each one offers a different approach, but they all share the same goal: giving your loved one safe, professional, and kind attention while you take a moment to breathe.
This flowchart can help you visualize the thought process—recognizing you're hitting your limit is always the first, most important step.
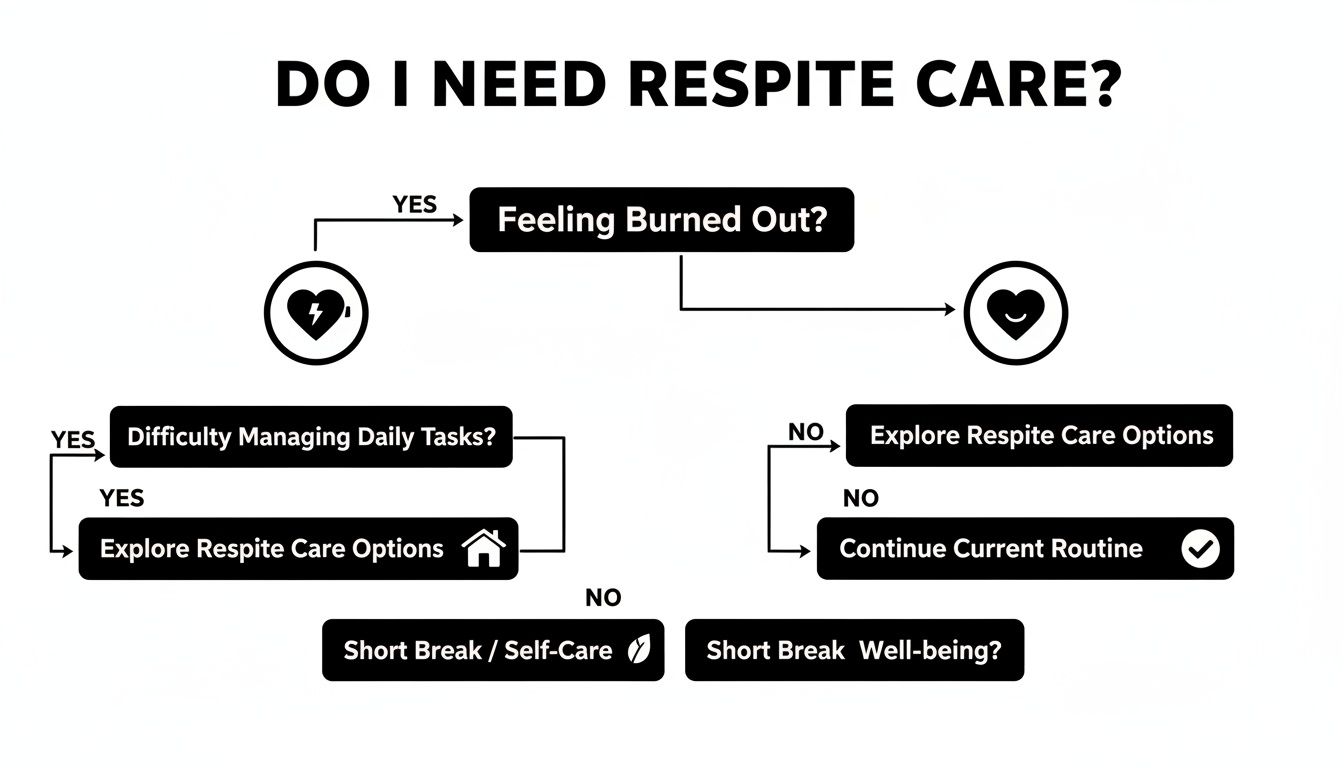
Ultimately, this is about acknowledging your own burnout so you can find and accept the help you deserve.
In-Home Respite Care
In-home care is just what it sounds like: a trained professional comes right to your house. This is often the best choice for someone with dementia because it allows them to stay in their own familiar, comfortable space. Keeping their routine as normal as possible is a huge help in reducing potential confusion and anxiety.
During a visit, an aide might help with personal care, make a meal, or just spend time looking through old photos or providing simple companionship while you're out.
- Best For: Individuals who get agitated in new places or have mobility issues that make going out a challenge.
- Pros: Maximum comfort and familiarity, one-on-one attention, and a flexible schedule.
- Cons: Can be more expensive than other options and doesn't offer the social buzz of a group setting.
Adult Day Centers
Adult day centers offer a structured, supervised environment for part of the day. They are a fantastic antidote to the social isolation that can creep in for both the person with dementia and their caregiver. These programs are built from the ground up to provide social connection and mental engagement in a safe place.
A typical day might include activities like music therapy, gentle exercise, art projects, and sharing a meal together. This not only provides a sense of community for your loved one but also gives you a predictable block of time for yourself.
An adult day program is like a bridge between living at home and moving into full-time care. It delivers the social and therapeutic perks of a community while letting your loved one return to their own bed each night.
These centers are staffed by professionals who are specifically trained in dementia care. They know how to manage challenging behaviors and create positive, uplifting experiences. If this sounds like a good fit, you can learn more about adult day care programs and what they offer.
Short-Term Residential Stays
Sometimes, a few hours just won't cut it. Maybe you need to travel for work, take a real vacation, or even recover from a medical procedure of your own. That’s where a short-term or overnight stay at an assisted living or memory care community comes in, providing 24/7 care for a few days or even a couple of weeks.
During their stay, your loved one essentially becomes a temporary resident. They get round-the-clock supervision, help with daily tasks, meals, medication management, and the chance to join in on social events with other residents.
This option offers complete peace of mind, knowing that trained staff are always on hand. It can also serve as a gentle "test drive" if you've been considering a future move to a residential community.
Comparing Respite Care Options for Dementia Patients
Choosing the right type of respite care can feel daunting, but breaking it down by features can make the decision much clearer. Each option offers unique benefits, and the best fit truly depends on your loved one’s needs and your family's circumstances.
This table provides a quick side-by-side comparison to help you weigh the pros and cons of each model.
| Feature | In-Home Care | Adult Day Center | Short-Term Residential Stay |
|---|---|---|---|
| Environment | At home, familiar surroundings | Community-based facility | Assisted living or memory care community |
| Social Interaction | One-on-one with caregiver | Group activities, peer socialization | Community life, group dining & events |
| Schedule Flexibility | Highly flexible, scheduled by the hour | Fixed daily/weekly schedule | Pre-booked for days or weeks |
| Level of Care | Companionship, personal care | Supervised activities, some personal care | 24/7 medical and personal care |
| Best for Caregiver | Running errands, short breaks | Predictable workday breaks | Vacations, travel, personal recovery |
| Best for Loved One | Prefers routine, has mobility issues | Craves social engagement, is mobile | Needs 24/7 supervision, trial for a future move |
Ultimately, there is no single "best" choice—only the best choice for you. Whether it's the comfort of home, the energy of a day center, or the security of a residential stay, the right respite care will provide the support your loved one needs and the break you've earned.
Recognizing the Signs of Caregiver Burnout
As a caregiver, it’s incredibly difficult to admit you need a break. We often tell ourselves that asking for help is a sign of weakness, but I can tell you from experience, that couldn’t be further from the truth. Caregiver burnout isn't just a possibility; it's an almost inevitable outcome when you're pouring so much of your physical, mental, and emotional energy into someone else.
Recognizing the signs is the first, most crucial step. It’s not about giving up; it’s about acknowledging your own limits so you can keep being there for your loved one. Ignoring these red flags just pushes you closer to a crisis point, where both your health and your ability to provide care are seriously at risk.

Key Red Flags to Watch For
Burnout is so much more than just feeling tired. It’s a deep, pervasive state of exhaustion that seeps into every corner of your life. These symptoms often creep up slowly, which makes them dangerously easy to dismiss at first. See if any of these sound familiar.
- Emotional Exhaustion: You feel constantly on edge—irritable, anxious, or maybe even depressed. Little things that you used to handle with ease now feel like monumental tasks, and you might find yourself snapping at people or feeling overwhelmed with frustration.
- Physical Depletion: You’re dealing with a bone-deep fatigue that no amount of sleep seems to fix. Maybe you're also getting more headaches, having stomach issues, or noticing big changes in your appetite or sleep patterns.
- Social Withdrawal: You’ve started pulling back from friends, family, and the hobbies you once loved. The idea of going out for dinner or catching up with a friend feels more like a chore than a pleasure.
Many caregivers say they feel like an "invisible second patient." It’s no wonder—over 11 million Americans provide more than 18 billion hours of unpaid care each year for someone with dementia. The personal toll is immense.
A Relatable Story
Maria had been caring for her husband, Tom, for three years after his dementia diagnosis. She took pride in being his rock, managing everything from his appointments and meals to his daily needs without a single complaint. But lately, she started waking up with a knot of dread in her stomach and found herself getting short with her daughter on the phone.
The breaking point came when she skipped a close friend's birthday lunch simply because she felt too drained to leave the house. That night, it hit her: she hadn't had a real, meaningful conversation with anyone but Tom in over a week. She felt completely alone. It was in that quiet moment she understood that taking care of herself wasn't a luxury—it was a necessity.
Taking Action Is a Sign of Strength
If you see these signs in yourself, please know that acknowledging them is a powerful act of self-preservation. Seeking respite care for dementia patients isn't selfish. It’s a responsible and vital step to protect your own health so you can continue your caregiving journey. For families wanting to learn more, understanding the deep connection between health and wellness in senior care can offer some valuable perspective. Acting before you hit a wall ensures you can return to your loved one with the renewed patience, energy, and love they deserve.
How to Choose the Right Respite Care Provider
Handing over the care of your loved one is a huge decision, and it’s one that calls for real diligence and a bit of homework. Choosing respite care for dementia patients isn't just about booking a room; it’s about finding a true partner who gets the unique world of memory loss. The right provider will do more than just keep your loved one safe—they’ll enrich their life while you get that much-needed break.
The absolute key is to find providers with specialized dementia training. General caregiving skills just don't cut it when you're navigating the complexities of cognitive decline, whether it's confusion, anxiety, or other challenging behaviors. Think of it this way: you wouldn't take a classic car to a generic oil-change shop. You’d go to a specialist who knows its specific quirks inside and out.
Start with a List of Questions
Before you even pick up the phone or schedule a visit, get a list of questions ready. Having them written down helps you compare apples to apples and keeps you from forgetting something critical in the moment.
Here are a few non-negotiables to get you started:
- Dementia-Specific Training: What kind of initial and ongoing training does your staff have specifically for dementia and Alzheimer’s?
- Staff-to-Patient Ratio: What’s the ratio of caregivers to residents during the day? What about at night? A lower number means more individual attention.
- Managing Challenging Behaviors: How do you approach situations like agitation, sundowning, or wandering? Ask them to walk you through a real example of how they de-escalate things.
- Communication with Families: How will you keep in touch with me while my loved one is with you? How often can I expect an update?
The answers you get should feel detailed, confident, and compassionate. They give you a direct look into a provider's expertise and their whole philosophy on care.
What to Observe During a Tour
A website can paint a pretty picture, but an in-person tour tells the real story. When you walk through a day center or a residential community, use all your senses. Your gut feeling is just as important as the checklist in your hand.
Keep an eye out for these tell-tale signs:
- Staff Engagement: Do the caregivers seem genuinely happy and connected with the residents? Watch how they speak to people—is their tone respectful, patient, and warm?
- Cleanliness and Safety: Does the place look and smell clean and well-cared-for? Look for safety measures like secured exits, clear hallways, and easy-to-use bathrooms.
- Resident Activity: Are people engaged and active, or are they mostly sitting around passively? A good community will have a nice balance of structured activities and quiet time.
The atmosphere of a place says everything. A truly great provider creates a space that feels warm, safe, and alive—a place where residents aren't just being watched, but are truly known and respected as individuals.
For instance, a specialized program like the one at Forest Cottage Senior Care is built to feel like a home, not a clinic. The staff knows every resident's name and story, fostering a sense of family that is so important for someone living with dementia.
Making the Final Choice
After you've done your research and taken your tours, give yourself time to sit with it all. Compare your notes and really think about which place fits your loved one's personality and specific needs. It's not just about finding a safe place; it's about finding the right place.
Ultimately, choosing a respite care provider comes down to trust. You’re looking for a team that not only has the right credentials but also shows a deep, compassionate understanding of dementia. To get a clearer picture of what a truly dedicated environment looks like, it can be helpful to explore what to expect from a memory care facility. Knowing what to look for will empower you to make the best possible decision for your family.
Navigating the Costs and Financial Aid for Respite Care
For most families, the decision to look for respite care is quickly followed by one big question: "How are we going to pay for this?" The financial side of dementia care can feel overwhelming, but figuring out the costs and what help is available is the first step to making this vital support a reality.
The price of respite care for dementia patients changes a lot based on the type of care, how long it's needed, and the level of support required. In-home care is usually billed by the hour, adult day centers often have a daily rate, and a short-term stay in a residential community will come with a daily or weekly fee that covers room, meals, and 24-hour care. Thinking about these costs upfront helps you build a realistic plan that fits your family's budget.
Breaking Down the Financial Landscape
The financial weight of dementia care on families is no small thing. In the United States, the total annual cost of dementia is a massive $781 billion. Even with Medicare and Medicaid covering significant parts of that, families still end up paying an estimated $52 billion out-of-pocket each year. These numbers really drive home how important it is to find and use every financial resource you can.
The good news? You don't have to carry this weight all on your own. There are several programs and organizations out there specifically designed to lighten the financial load for caregivers, making respite care much more attainable.
Key Sources of Financial Assistance
Figuring out the world of financial aid can feel like a maze, but knowing where to start is half the battle. Many families are actually eligible for support they don't even realize exists. Here are the main places to look for financial help.
- Medicare: Original Medicare (Part A and B) usually doesn't cover long-term custodial care. However, it might pay for short-term respite stays in certain cases, like under hospice benefits. Some Medicare Advantage (Part C) plans offer more coverage that could include in-home help or adult day care services.
- Medicaid: As a joint federal and state program, Medicaid is one of the biggest funders of long-term care. You have to meet certain income and asset limits to qualify, but for those who do, it can cover a wide variety of services, including respite care. The details change from state to state, so you'll need to check with your state's Medicaid program.
- Department of Veterans Affairs (VA): If your loved one served in the military, the VA offers some incredible support. Programs like the VA Aid and Attendance benefit can provide monthly payments to help with care costs. The VA also has its own respite care programs that can provide up to 30 days of care each year.
- Non-Profit Grants and Programs: Groups like the Alzheimer's Association provide grants through their Respite Care Grant programs. Your local Area Agency on Aging is another fantastic resource for finding grants and financial aid opportunities specific to your community.
Understanding your options is empowering. Don't just assume you won't qualify for help. Taking the time to look into these programs can unlock the support you need to make respite care a regular part of your caregiving routine.
Taking the Next Steps
The journey to getting financial aid starts with some research and asking the right questions. A great first step is to contact your local Area Agency on Aging—they act as a central hub for all things senior resources. They can give you personalized advice based on where you live and your specific situation.
If you're trying to understand how state programs like Medicaid can help with different kinds of senior living, our guide on whether assisted living is covered by Medicaid offers some valuable insights into the qualification process. By looking into each option one by one, you can start to piece together a financial plan that makes those much-needed, restorative breaks possible.
Preparing for a Positive Respite Experience
A good respite experience—whether it's for a few hours or a few days—starts long before you drop off your loved one. A little thoughtful prep work can make the transition much smoother for everyone, turning what could be a stressful event into a genuinely positive one.
When someone is living with dementia, easing into the process is almost always the best strategy. This might mean starting small. You could have an in-home aide come over for a short visit while you're still in the house, just to build a gentle rapport. For an adult day program, a half-day trial run can be a great introduction, letting them get a feel for the place without feeling overwhelmed.

Creating the "All About Me" Guide
One of the most powerful tools you can give the care team is a detailed information sheet. Think of it as a user manual for your loved one. This simple document helps the new caregivers see them as a whole person, not just as a patient.
Be sure to include these key details:
- Daily Routine: Note their typical wake-up time, meal times, and bedtime rituals. Consistency is comfort.
- Preferences: What are their favorite foods, music, or TV shows? What activities do they still enjoy?
- Communication Style: How do they best communicate? Do they respond better to simple, direct questions or visual cues?
- Triggers and Soothers: What might cause agitation, like loud noises? And just as important, what helps calm them down—a specific blanket, a favorite song, a quiet room?
This guide is your voice when you're not there. It helps the respite team provide personalized, compassionate care that honors your loved one's history and personality, making their stay much more pleasant.
Packing for Comfort and Familiarity
For any time spent away from home, packing familiar items is absolutely crucial. The goal is to make an unfamiliar space feel just a little more like their own. A well-prepared bag can make a world of difference in reducing anxiety.
Your packing checklist should include:
- Comfortable Clothing: Pack easy-to-wear outfits that are familiar and cozy. And don't forget non-slip socks or slippers.
- Familiar Items: A favorite blanket, a cherished family photo, or a well-loved pillow can provide an incredible amount of comfort.
- Toiletries: Even if the facility provides them, using their own toothbrush, soap, and lotion helps maintain their personal routine.
- Important Documents: Bring a copy of their insurance cards, a complete list of all medications (including dosage and timing), and, of course, your "All About Me" guide.
Preparing Yourself for the Break
Finally, remember this break is for you. It’s completely normal for caregivers to feel a messy mix of relief and guilt. Acknowledge those feelings, but please don't let guilt rob you of this essential time to recharge.
Remind yourself that respite care for dementia patients isn't giving up; it's a proactive strategy to sustain your own health so you can keep going.
Plan how you'll use your time. Whether it's sleeping in, meeting a friend for lunch, or just reading a book in total silence, be intentional about doing things that fill your cup. By truly resting and recovering, you can return to your caregiving role with renewed energy and patience—ready to provide the best possible care for the person you love.
Common Questions About Dementia Respite Care
Stepping into the world of respite care always brings up a lot of questions. It's completely normal to feel a bit uncertain when you're making such a big decision for your family. To help you feel more confident, we've put together clear, straightforward answers to the concerns we hear most often.
How Do I Handle My Loved One’s Resistance?
One of the toughest hurdles is when a parent or spouse resists the idea of a new person coming in to help. This is a very common reaction, and it usually comes from a place of fear—fear of the unknown, or not wanting to feel like a "burden."
The best approach is a gentle and gradual one. Instead of presenting it as “care for you,” try framing it as “help for me.” You could say something like, “I’ve found someone to help me with a few things around the house, and they can keep you company while I’m busy.”
Start with short, casual visits. Maybe the new caregiver can just join you both for a cup of tea or go for a short walk together. This low-pressure approach helps build familiarity and trust, allowing your loved one to see the caregiver as a friendly face rather than an intruder.
Think of it like introducing a new friend. When you focus on the positives, like having someone to chat with or do an activity with, you shift the focus away from the "care" part. That small change in language can truly make all the difference.
What Happens During a Medical Emergency?
This is, without a doubt, a top concern for every family. Any reputable respite care provider will have very clear and practiced emergency plans. Before care even starts, they should sit down with you to create a detailed care plan.
This plan needs to include:
- Emergency Contacts: A full list of family members, doctors, and anyone else who should be notified.
- Medical History: A clear summary of their health conditions, any allergies, and a current medication list.
- Advance Directives: Copies of important documents like a living will or a Do Not Resuscitate (DNR) order.
- Hospital Preferences: Your preferred hospital, so there's no confusion in an urgent situation.
Caregivers should be trained in basic first aid and CPR. In a serious medical event, their first move is always to call 911. Their second is to call you immediately. This two-step process ensures your loved one gets professional medical help right away while you're kept in the loop every step of the way.
How Often Should I Use Respite Care?
There really is no one-size-fits-all answer here—it all comes down to what you need. Some family caregivers find that a few hours once or twice a week gives them just enough time to run errands and catch their breath. Others might need a full day every week or even a whole weekend once a month to truly recharge.
The main goal of respite care for dementia patients is to prevent burnout, not just react to it. It’s always better to schedule regular, planned breaks before you hit a wall. Plus, having a consistent schedule is often better for your loved one, too, as it helps them get into a comfortable routine. Start with what feels right and don't be afraid to adjust as your needs change.
At Forest Cottage Senior Care, we know every family's situation is different. Our respite and senior day care programs are built to provide a safe, engaging, and warm environment for your loved one, giving you the time you deserve. To see how we can support your family, feel free to explore our care options at https://www.forestcottageseniorcare.com.